CBCT & Radilogy Protocol for Implant Diagnosis
- Introduction
- Imaging Modalities
- Requirements &Types of Imaging Modalities
- Imaging phases of dental implant therapy
- Conclusion
Introduction
-
Diagnostic imaging helps develop an appropriate and precise treatment plan for implant patients.

- Diagnostic imaging and techniques help develop and implement a cohesive and comprehensive
treatment plan for the implant team and the patient
Imaging Modalites:
- The variety of imaging modalities available vary from simple 2-Dimensional views such as panoramic radiographs to more complex views which allow image visualization in multiple planes.
Ideal diagnostic imaging depend on a number of factors:
- The amount of information required
- Period of treatment rendered
- Type of information required
Requirements of imaging modalities:
Any diagnostic imaging modality should ideally satisfy the following basic principles:
➢ adequate number and types of images should be obtainable in order to provide required anatomical information.
➢ the imaging technique selected should provide the accurate required information
➢ The images obtained should be with minimal distortion.
➢ if more than one imaging modality is feasible, the imaging information should be governed by the ALARA (As low as Reasonably Achieved) principle.
➢ It should be affordable for most patients.
Imaging phases of dental implant therapy:
PHASE 1: Presurgical implant imaging
- Involves all past radiologic examinations and new radiologic examinations to determine the patient’s final and comprehensive treatment plan.
Objectives:

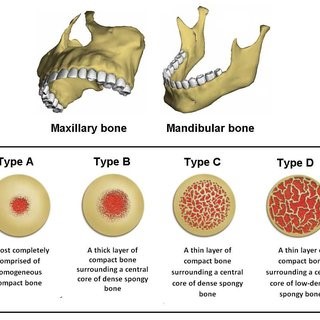
BONE Quantity, quality and angulations of bone
ANATOMY Relationship of critical structures to the implant site
PATHOLOGY The presence or absence of disease at the implant site
Imaging modalities:
➢ Conventional
Periapical radiography
-
It is produced by placing the film intraorally parallel to the body of the alveolus at the region of interest, producing the lateral view of the alveolus.
Bitewing radiography
Occlusal radiography
Cephalometric radiography
Panoramic radiography
ADVANTAGES:
- Easy identification of opposing landmarks.
- Initial assessment of vertical height of bone.
- Convenience, ease, and speed in performance in most dental offices.
- Evaluation of gross anatomy of the jaws and any related pathological findings.
LIMITATIONS
- Distortions inherent in the panoramic system.
- Errors in patient positioning
- Does not demonstrate bone quality.
- Misleading quantitate because of magnification and no third dimension
- No spatial relationship between structures.
Limitations of conventional radiography:
2 D Superimposition Contrast Difference Adjustment
➢ Advanced
Magnetic resonance imaging

Conventional tomography
Conventional tomography
Computed tomography
- The individual element of the CT image is called a voxel, which has a value, referred to in Hounsfield units, that describes the density of the CT image.
- The density of structures within the image is absolute and quantitative and can be used to differentiate tissues in the region.
Indications:
- Interactive treatment planning

- Determination of bone density
- Vital structure location
- Sub periosteal implant fabrication
- Determination of pathology
- Preplanning for bone augmentation.
Advantages:
- Negligible magnification
- Relatively high-contrast image
- Various views
- Three-dimensional bone models
- Interactive treatment planning
Limitations:
- Cost
- Technique sensitive.
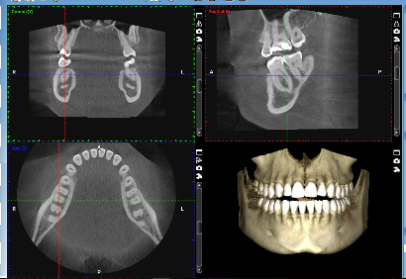
Cone beam computed tomography
(Third Eye in Dentistry)
How is the image produced?
Axial Plane
Coronal Plane
Coronal Plane slices through the anatomy from side to side.
Sagittal Plane
Sagittal Plane is a slice through the anatomy from front to back
Series of Cross-sectional/Transaxials
Cross sectional images of an area can be developed with .5 to 5mm spacing between images.
Objectives Presurgical implant imaging:
- To determine the quantity, quality and angulations of boneAfter adequate height is available, the next most significant criterion affecting long-term survival of implants is the width of the available bone
- Determine relationship of critical structures to the implant site.
 Anterior Maxillary Superior Artery
Anterior Maxillary Superior Artery- Naso –Palatine Canal
- Inferior Alveolar Canal
- Mental Foramen
- Anterior Loop
- Maxillary sinus
PATIENT Evaluation:
- Evaluation of the implant patient should be disciplined and objective
- The objectives for any radiographic evaluation, regardless of imaging technique used, should include an evaluation to
- Exclude pathology,
- Identify anatomic structures, and
- Measure the quantity, quality, and location of available bone

PHASE 2 Surgical and Intraoperative implant imaging:
- Focused on assisting in the surgical and prosthetic intervention of the patient.
- Objectives
- To evaluate the surgical site during and after surgery
- Assist in the optimal position and orientation of dental implants
- Evaluate the healing and integration phase of implant surgery
- To ensure that abutment position and prosthesis fabrication are correct.
- With digital radiography technology, instantaneous images are achieved, allowing for multiple images to be completed in a fraction of the time
PHASE 3 Post prosthetic implant imaging:
- It commences just after the prosthesis placement and continues as long as the implant remains.
- Objectives
- To evaluate the long term maintenance of implant rigid fixation and function, including crestal bone levels
- To evaluate the implant complex.
- Implants should be radiographically assessed on an annual or biannual basis. In the implant’s first year of service, annual vertical bone loss be less than 0.2 mm is normal.
Choice of radiographic technique:
- 1. For asymptomatic implants:
- Intraoral periapical
- Panoramic imaging in extensive cases
- CBCT is not indicated for periodic review of asymptomatic implants
- 2. CBCT imaging
- Implant mobility
- Altered sensation
- Implant retrieval Periapical Radiographs
- Peri-implant radiolucency indicating bone loss: (2mm of loss is acceptable in the first year, and 0.2mm each year after)
- Widening of the PDL space of adjacent natural teeth which indicates poor stress distribution
- Evidence of saucerization indicating loss of crestal bone
- Apical migration of the alveolar bone or indistinct osseous margins.
Examination of Implant Failures and Complications Using CBCT
A. Altered sensation:
- disturbance to the mandibular canal
- Damage to the nasopalatine canal
B. Infection or postoperative integration failure.
C. Perforation:
- Perforation of the lingual bone plate in the anterior mandible and resulting severe hemorrhages and life-threatening airway obstructions.
- Perforation of the floor of the nose during implant bed preparation and/or placement→ difficulty in breathing and infection ant tip may be shortened until soft tissue coverage is attained.
Conclusion:
- Many radiographic projections are available for the evaluation of implant placement, each with advantages and disadvantages
- The clinician must follow sequential steps in patient evaluation, and radiography is an essential diagnostic tool for implant design and successful treatment of the implant patient “as low as reasonably achievable” (ALARA)


